
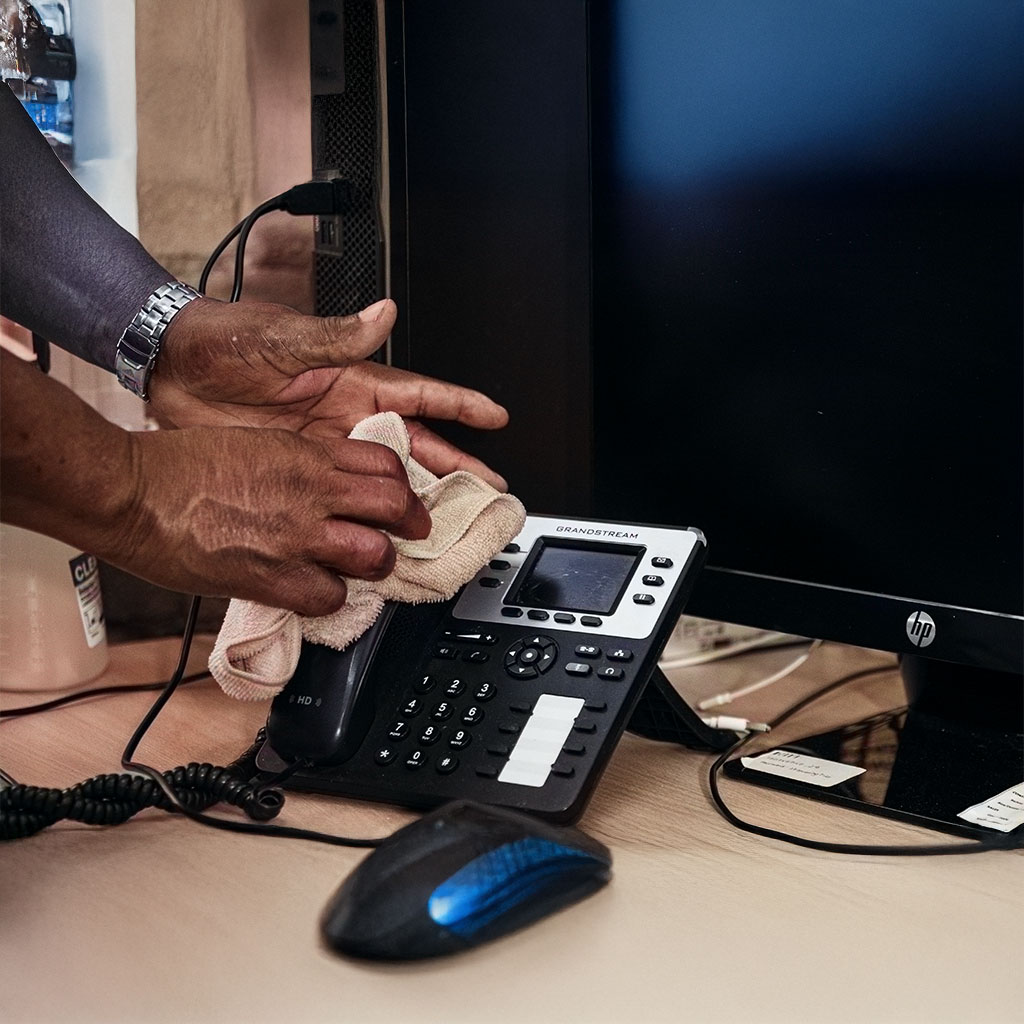
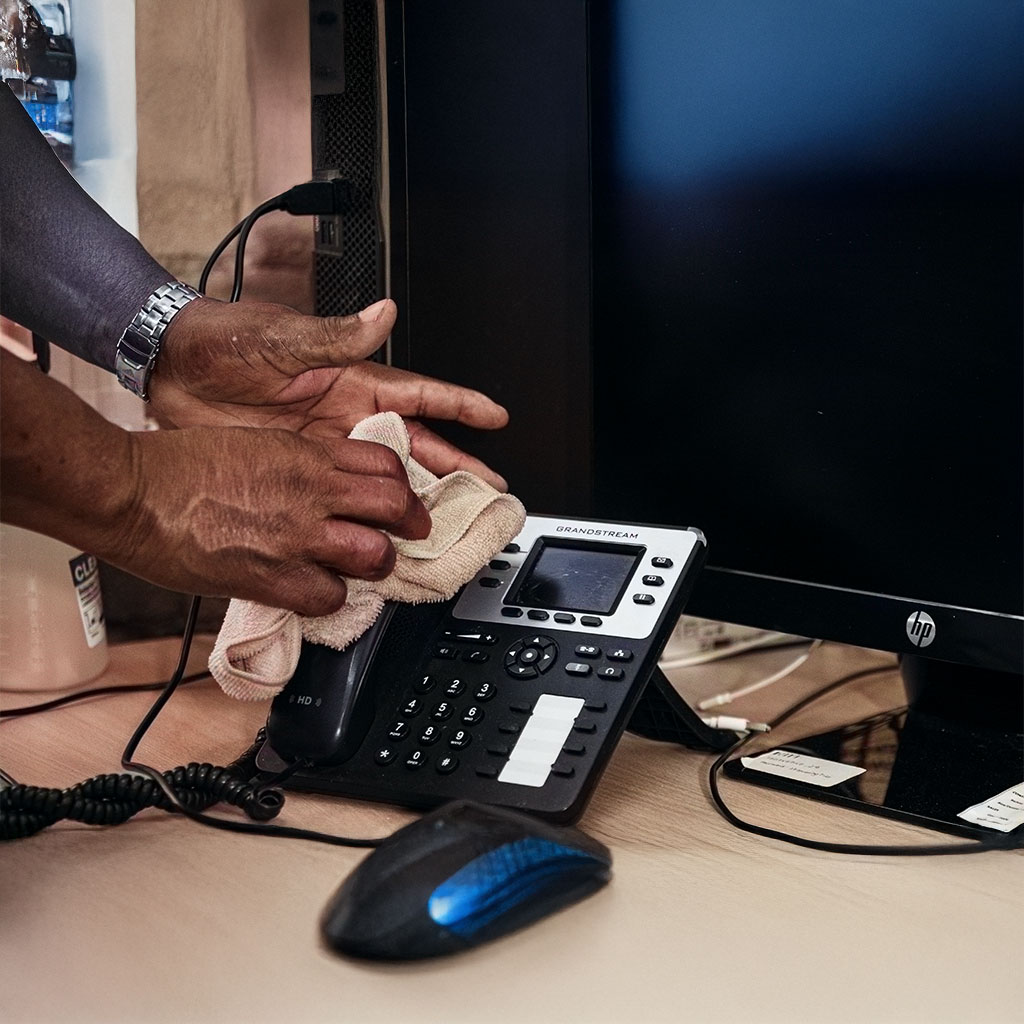
Cleaning a medical facility such as a dispensary, hospital, clinic, or emergency care centre is a critical responsibility.
All these facilities require far higher standards of cleanliness and compliance than other industries.
A clear reason is that a lot of patients, each with their own illness or disease, may contract healthcare-associated infections (HAIs).
An in-house cleaning team might be a good choice if the team knows the medical-facility cleanliness standards; otherwise, it’s a poor choice.
Here comes the medical facility cleaning services in the UK, which is the safest option. Let’s learn why.

First, let’s talk about the main cleaning standards that must be followed in any healthcare sector:
These standards set how healthcare facilities plan, do, and prove cleaning. They use Functional Risk (FR) categories and a public star-rating to show results. They also set how audits work and how teams record evidence. The 2025 update applies across NHS organisations and replaces the 2021 version. (NHS England)
The NHS National Standards of Healthcare Cleanliness 2025 set six Functional Risk (FR) categories. Each FR level has a target audit score and a suggested audit frequency. FR1 is the highest risk and needs the tightest standard; FR6 is the lowest and needs less frequent checks.

FR1 – Very high risk
98%+, weekly audits. Used where infection risk is greatest. Examples often include ICUs and theatres in older guidance. Always confirm locally.

FR2 – High risk
95%+, monthly audits. Think of busy clinical areas with frequent procedures.

FR3 – Medium risk
90%+, every 2 months. Long-stay wards, or treatment centres are common examples in prior materials. Check your trust’s mapping.

FR4 – Lower-medium risk
85%+, every 3 months. Outpatient-type spaces are typical but confirm locally.
FR5 – Low risk
80%+, every 6 months. Often in admin or back-office areas.
FR6 – Very low risk
75%+, every 12 months. Storage or non-clinical spaces.
Why this matters: the higher the FR, the more often you clean and audit, and the higher the score you need. Those scores roll up into your public star rating, so keeping clear evidence and delivering stable results will pay off.
Not to follow blindly: NHS gives the table above as a guide. Organisations may set a different frequency if that better protects patients. Review your schedule often.
Choose the right FR for each area: Start by mapping every room to the proper FR. Your trust policy should list examples for each FR and how to audit them.
The National Infection Prevention and Control Manual is an evidence-based, step-by-step guide. It is mandatory in NHS settings, and its core Standard Infection Control Precautions (SICPs) apply in all care settings. Use it to train staff and write simple, clear SOPs. (NHS England)
Standard Infection Control Precautions (SICPs) are the everyday safety habits used with every patient, every time, because you can’t always tell who might be infectious. Think of them as your baseline routine:
Bottom line: assess the task, pick the right precautions, do them every time, and record what matters. Make SICPs a habit, not a hassle.
Care Quality Commission (CQC) is the independent regulator of health and adult social care services in England. It checks if you assess, manage, and control infection risk, and how you share concerns. For adult social care, CQC also provides an information-gathering tool to help you show evidence. Keep policies, logs, and actions easy to find. (cqc.org.uk)
NICE QS61 is a 2014 UK National Institute for Health and Care Excellence (NICE) Quality Standard for preventing and controlling healthcare-associated infections in adults, young people, and children across primary, community, and secondary care settings.
It outlines specific, measurable statements for high-quality care and includes quality measures focusing on antimicrobial stewardship, hand hygiene, urinary catheters, vascular access devices, and education on infection control.
NICE QS61 lists short, clear quality statements for safe care. Map your audits, training, and reviews into these statements so leaders can track progress. (NICE)
Staff follow strict Control of Substances Hazardous to Health (COSHH) in a medical facility when storing, using, and reviewing cleaning and disinfectant chemicals. Trained staff to use the right PPE and keep Safety Data Sheets and risk assessments up to date.
When you claim a disinfectant “works,” show the right EN test: EN 1276 (bactericidal), EN 13697 (surface test), EN 14476 (virucidal), and EN 16615 (disinfectant wipes, “4-field” test). File the certificates with your SOPs. (BSI Knowledge)
| Standard | Target (bacteria/virus/fungi) | Typical use case (surface/wipe/solution) | Evidence to file |
|---|---|---|---|
| EN 1276 | Bacteria | Solutions for general disinfection (after cleaning) | Current certificate/test report |
| EN 13697 | Bacteria, yeasts/fungi (surface test) | Hard non-porous surfaces | Current certificate/test report |
| EN 14476 | Viruses | Medical-area disinfectants | Current certificate/test report |
| EN 16615 | Bacteria/yeasts (wipes, 4-field) | Wipes/mops with mechanical action | Current certificate/test report |
Use the standard that fits the task and keep proof with COSHH and SOP packs.
Hospitals, GP surgeries, dental practices, community clinics, and care homes all use this mix. The NHS standards set the cleaning framework; the NIPCM gives daily steps; CQC checks outcomes; NICE guides quality; HSE/COSHH keeps chemical use safe. (NHS England)
HTM Specialisations in Medical Facility You Can’t Ignore (01-01, 01-05, 01-06, 07-01)
Some rooms need extra rules. This is where Healthcare Technology Management (HTM) comes in. It falls under four categories:
Use these with the NHS 2025 cleanliness standards: keep your FR mapping and audits, then layer the HTM steps for theatres, dental rooms, endoscopy suites, and waste areas. NHS England
Your compliant cleaning process should be “simple, clear, repeatable. So, follow these to get best cleaning outcomes:
Split the building into zones (wards, clinics, waiting areas, offices). In each room, list the high-touch points (bed rails, chair arms, door handles, keyboards, taps).
Give every room an FR level (FR1–FR6). Higher risk = clean more often and audit more often. Post your star rating where people can see it.
use detergent to remove dirt and then disinfectant when the risk says so. Keep the surface wet for the full contact time shown on the label.
Follow colour-coding (e.g., red for washrooms, blue for general areas). Don’t move mops and cloths between zones.
Show which PPE to wear for each task. Teach donning/doffing the right way.
Keep equipment logs: what was used, where, when, and by whom. Swap heads and clothes at the right times.
After discharge or when isolation ends, do a terminal clean. Your IPC team can help set the trigger and steps.
Build everything to the NHS 2025 standards: FR categories, audits, and star ratings. Keep it simple. Keep it visible.
You need proof that your plan works day-to-day. Keep it neat, dated, and easy to find.
People & Skills
Think of this as your “who and how trained” section.
A recent national point-prevalence study found notable levels of Healthcare-Associated Infections (HCAIs) in England. Strong cleaning, good records, and regular reviews help reduce risk and show regulators that you are in control.
Keep a 90-day pack ready: last 3 months of audits, actions, training updates, and star-rating sheets, plus COSHH and product certificates.
Clean more when the area gets used a lot, and less when it’s not as busy. Nights and weekends can get busy, too. If patient flow rises, raise the FR level or add extra rounds. Write down what changed and why. Make sure handovers are clear: who cleans what, when, and with what product.
Some products need a wet contact time (the surface must stay wet for the full minutes on the label). Others work in a shorter, “dry” window or as a wipe with a tested method. If it dries too soon, you may not get the kill you expect. Keep a simple “contact-time cheat sheet” on the trolley. Do not wipe dry early.
Anything that moves between patients or rooms can spread germs: pumps, cuffs, remotes, keyboards, touch screens. Give each item a quick between-use wipe and a daily deeper clean. Use colour-coding so the kit from bathrooms never touches clean areas.
If a partner helps with cleaning, make sure they follow your FR map, your SOPs, and your products. Do a short induction, check training and COSHH, and agree on audit and CAPA rules. Keep proof: who was on shift, what was cleaned, and any fixes made. One page is enough if it’s clear.
Verify supplier claims. Use UKAS CertCheck to confirm ISO/EN certificates and lab claims before you accept them. It’s free and public. (ukas.com)
UKAS is the UK’s National Accreditation Body, appointed by the government to assess and accredit organisations that certify and test.
Here is the Provider selection checklist you can use and ask questions during your first session:
As a leading medical facility cleaning services UK, we do clean with strict compliance first and patient safety:
At Innovative Cleaning Services, we make it simple to prove that cleaning is being done right, on time, and to standard for your medical facility.
Get a free compliance walkthrough. We’ll map your FR categories, review chemicals and COSHH, and deliver a risk-based proposal with timelines and an evidence pack you can use in audits.
Cleaning a medical facility is far more demanding than cleaning other facilities. All regulations must be followed.
Some medical facilities are aware of these regulations, while some find them challenging to implement, which is why our healthcare cleaning services in the UK exist.
We follow the National Standards of Healthcare Cleanliness 2025, Functional Risk (FR) categories, and the National Infection Prevention and Control Manual (NIPCM).
We deliver IPC cleaning services in the UK with EN 14476-tested products, colour-coded cleaning equipment, proper checklists and clear audits.
As hospital cleaning contractors, we help make compliance visible and easy for everyone through our clinical cleaning services in the UK.
23% of hotels and 16% of guesthouses reported using eco-friendly cleaning products. Though…
Home Gym cleaning is an important part of gym facility maintenance. Your…
Home School is a vast place with complex structures. Hundreds of classrooms,…
Home Since the advent of AI, industries have experienced significant makeovers, both…
Home Your office is where your financial and marketing and HR operations…
Home You are a store manager or maybe the person responsible for…
Home Cleaning a medical facility such as a dispensary, hospital, clinic, or…
You might choose a bargain commercial cleaning company that could make your…